Operating Room Team
When a patient is about to undergo a surgical procedure direct patient care will be pass on to the operating room personnel. The operating room (OR) team is responsible for the well-being of a patient throughout the operation. This team should not only consider the patient’s privacy but will also promote safety measures for the patient. One way of promoting safety of patients inside the OR is by preventing infection from the surgical incision that will be done.
As described, the OR team is similar to that of a symphony orchestra. There are many members in an orchestra but they work together in unison and harmony to create a superb outcome. The operating room (OR) team does the same thing. They coordinate their work with each other to have a successful operation.
Classification of OR team
There are two types of OR team according to the functions of its members.
- Surgeon
- Assistants to the surgeon
- Scrub person (either a registered nurse or surgical technologist)
- Anesthesiologist
- Circulator
- Biomedical technicians, radiology technicians or other staff that might be needed to set up and operate specialized equipment or devices essential in monitoring the patient during a surgical operation
Operating Room Team: Sterile Personnel
The members of the OR sterile team will do the following things:
- Perform surgical hand washing (arms are included).
- Don sterile gowns and gloves.
- Enter the sterile field.
- Handles sterile items only.
- Functions only within a limited area (sterile field).
- Wear mask.
Operating Surgeon
The surgeon is a licensed physician (MD), osteopath (DO), oral surgeon (DDS or DMD), or podiatrist (DPM). This professional is especially trained and is qualified by knowledge and experience for the performance of a surgical operation.
Responsibilities of a surgeon:
- Preoperative diagnosis and care of the patient
- Performance of the surgical procedure
- Postoperative management of care
Assistants to surgeon
During a surgical procedure, the operating surgeon can have one or two assistants to perform specific tasks under his/her (operating surgeon) direction. The responsibilities of a surgeon’s assistant:
- Help maintain the visibility of the surgical site
- Control bleeding
- Close wounds
- Apply dressings
- Handles tissues
- Uses instruments
Types of Assistants to Surgeon:
- First Assistants could either be:
- A qualified surgeon or resident in an accredited surgical education program. The first assistant should be capable of assuming the operating surgeon’s responsibility in cases of incapacitation or accidents.
- Registered Nurse and surgical technologists that have a written hospital policy permitting the action.
- Second Assistant could be a registered nurse or surgical technologist. These staff should be trained and they mar retract tissues and suction body fluids to help provide exposure of the surgical site.
Scrub Person
A scrub person could be the following:
- Registered Nurse
- Surgical technologist
- Licensed practical/vocational nurse
The responsibility of a scrub person is to maintain the integrity, safety and efficiency of the sterile field throughout the surgical procedure.
Purposes of Surgery
1. Diagnostic – establish the presence of disease condition
2. Exploratory – determine the extent of disease condition
3. Curative – treats the disease condition
ABLATIVE – removal (EG: Appendectomy)
CONSTRUCTIVE – repair of Congenital defects (EG: Cheiloplasty)
RECONSTRUCTIVE – repair of damaged organ
4. Palliative – placement of PEG tubes for Stomach Cancer
Magnitude of Surgery
MAJOR – High risk for Cx; (EG: Craniotomy, Explore Lap)
MEDIUM – (EG: appendectomy, hemorrhoidectomy)
MINOR – decreased Cx is involved (EG: Excision, Removal of ingrown)
Urgency
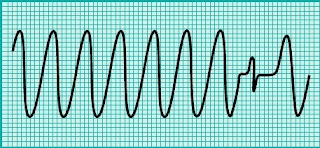
Emergency – done immediately. Hemorrhage, VA
Imperative – done within 24-48° Gangrene, Amputation
Planned – in weeks or months Thyroidectomy, MRM
Elective – delay will not cause adverse effects Cauterization of warts, Lumps
Optional - requested by the client; for Aesthetic purposes Rhinoplasty, Blepharoplasty
PRE OP Assessment
Prepare patient at least a day before
Age
Pain (Presence vs Tolerance)
Nutritional status
Hydration (IVF 1° prior to Surgery)
Infection (prophylaxis @ least 1° before Sx thru IV push; Skin Testing is done b4 giving)
Operation time:
ATBC or other drugs given?
Skin testing for allergic reaction
Medications
STOP ASA at least 1 week before the Surgery to avoid bleeding
Current drug therapy
Allergy
Others
Prepare 3 units of blood prior to Surgery
Religion (not allowed if pt is Jehovah’s witness)
Occupation (post insertion of Harrington rod, he can no longer bear heavy objects)
SO (close relationships)
Review of Systems (for clearance)
Hematologic = CBC, Hct, Hgb
Pulmonary = Far advanced PTB, Asthma
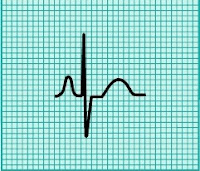
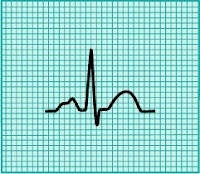
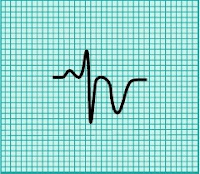
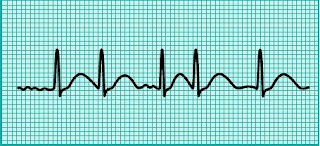
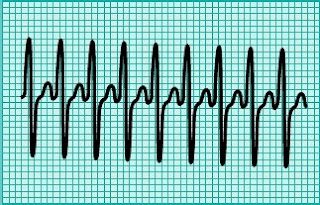
Cardiovascular = pacemakers
Neurological = hemiphlegia
Renal = status post kidney transplant; BPH
GI = Ulcers because NPO is instructed
Endocrinological = BSL defers Sx; CBG q1°
Reproductive
CONSENT
- valid only for 24° only
- pt understands the nature of the Tx, potential Cx, alternatives
- w/o pressure; voluntary
- protection against legal action
PREPARATIONS
PRE-OP Rounds
- skin test
- personal hygiene – the night before
- diet = Liquid, NPO
- bowel – abdominal Sx = bowel prep; Cleansing enema
- skin Ortho prep (sa OR); Skin prep (shaving only)
- IV Line
INTRA OP
- Verification
- Quick assessment
POST OP
exercise (DBE)
Contraptions – Abdominal: NGT, IVF, O2
Explore lap: NGT
Miscellaneous
40 y/o & above – needs Cardiovascular clearance
Clearance from Attending Physician
Monitoring VS of pts
Check op site
Blood request (SOP: 2 units of blood)
Bill settlement
Expectations
Possible Complication
Health teachings: Abd Sx (Teach DBE & Side lying position = Adhesionlysis)
Limitations: Hip prosthesis (do logroll)
IMMEDIATE POST OP (post anesthesia recovery stage)
EXTENDED POST OP